Red Flags And Preventative Action
"I have this tingling sensation in my feet all the time. What's wrong?"
"My feet feel like they are burning. What's going on?"
"My foot has felt numb for a while and the feeling hasn't come back. What's happening?"
These are common questions we hear from new patients in diabetic foot treatment who are in the early stages of diabetes. Some patients are not yet aware they have diabetes because symptoms in the past have been so subtle they have not felt the need to seek medical advice.
This is not uncommon. The American Diabetes Association estimates there are 7.3 million Americans struggling with health problems related to undiagnosed type 2 diabetes with another 1.5 million Americans newly diagnosed each year.
This article shares the physical symptoms signaling you are at risk for developing diabetic foot ulcers and immediate steps you can take to stop foot sores from forming.
The good news is, early detection and treatment of type 2 diabetes can decrease the risk of developing diabetic foot wounds. Patient education, compliance and a well-integrated, multi-specialist care team is key to protecting feet and overall health.
"Am I At Risk Of Losing My Foot?"
That is the most common fear patients have when they start losing feeling in their feet. This series of blog articles addresses those fears along with the most common questions and concerns that patients and their families have regarding diabetic foot wound prevention, diabetic wound healing and successful limb sparing procedures.
If you or someone you love is experiencing numbness, redness, swelling or sore places that aren't healing on the feet, you should take a few minutes to read through this list of steps that should be taken to address "at risk" indicators during an initial patient assessment with a diabetic foot specialist.
What Part Of The Body Does Diabetes Affect First?
Skin concerns are usually the first significant problem that motivate people to seek medical advice and most skin issues are caused by damaged blood vessels. By the time skin issues become obvious, damage to the microvascular arterial flow has already occurred due to uncontrolled blood sugar. Arteries and blood vessels in the legs become narrowed or blocked, this is diagnosed as peripheral arterial disease (PAD). These damaged arteries aren't able to supply adequate blood and oxygen to the smaller blood vessels that nourish nerves and soft-tissue of the foot.
Diabetes can also cause nerve damage known as peripheral sensory neuropathy. We all put significant pressure on the skin of our feet from carrying our body weight all day. People with peripheral neuropathy may not feel pain from increased pressure areas on their feet causing skin breakdown. This is referred to as micro-repetitive trauma.
What Is An "At Risk" Foot For Developing Ulcers On The Feet?
An "at risk" foot is commonly referred to in diabetic foot wound care terms as Stage 2, Grade 0.
In diabetic foot treatment programs, standardizing communication among multiple specialists caring for the patient is important to facilitate optimal, integrated care. There are two widely accepted methods of communicating the "stage" of the diabetic foot as a whole, as well as classifying the "grade" of each individual wound as it heals during the course of treatment. You may hear your providers using these terms during your care and might see them noted in your medical records and reports.
There are six diabetic foot stages beginning with Stage 1 - normal foot, no risk factors, to Stage 6 - a foot that cannot be rescued. Individual wounds are also classified and the most commonly used is the Wagner-Meggitt classification. It includes a range of five diabetic wound grades starting with Grade 0 - skin is intact, but bony deformities of the foot and ankle lead to "at risk" foot, to a Grade 5 - extensive gangrene.
In this article we address the Stage 2 diabetic foot with a Wagner-Meggitt classification of 0. Stage 2 is categorized as high risk for ulceration. In Stage 2, the foot has developed one or more of the following risk factors for ulceration: neuropathy, ischemia (inadequate blood supply), structural deformity, swelling, or a corn or callus,
Five Main Indicators For Risk
When an early diabetic patient presents to our practice with any of the above complaints, our diabetic foot specialist evaluates five main indicators to assess where the patient is on the Stage 2 spectrum.
Indicator 1. Are the dorsalis pedis and the posterior tibial arteries palpable?
By physical assessment, your doctor will conduct a vascular exam by palpating the dorsalis pedis artery on the top of the foot and the posterior tibial artery at the back of the ankle.

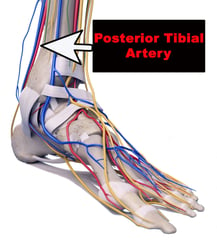
If your doctor can feel strong, normal pulses at both arteries then they know circulation to the foot is healthy and there is no need to access circulation any further.
If they cannot feel a strong pulse they will schedule an Arterial Doppler Study with ankle brachial index in our office. Ankle brachial index (ABI) compares the systolic blood pressure from both brachial arteries (the brachial artery is the major blood vessel supplying blood to the upper arm, elbow and forearm) with both the dorsalis pedis and posterior tibial arteries in the foot and ankle. ABI has been shown to be a specific and sensitive metric for the diagnosis of Peripheral Arterial Disease.
The major cardiovascular and diabetes societies recommend measuring an ABI at least annually for every smoker and every diabetic patient over 50 years of age and adults over the age of 65.
As our physician is completing the physical exam they are also taking a medical history. Because of the symptoms presented above, this medical history interview includes a quick screen to identify other symptoms of diabetes in patients who have not been previously diagnosed. Questions include:
- How frequently are you urinating during the day? How frequently at night? Urinating more than seven times during the day and once or twice at night may be a sign kidneys are working overtime to flush out excess sugar in the blood.
- Do you feel thirsty all the time? How many glasses of water are you drinking a day? If it's more than a gallon (16 eight ounce glasses) of water a day and you still feel thirsty, this is another sign of high blood sugar. Kidneys are working overtime to filter and absorb the excess glucose. When the kidneys can't keep up, excess glucose is excreted into urine, dragging along fluids from tissues, which causes dehydration and thirst.
- How many times a day are you eating? Is that more than usual? Do you still feel hungry after eating a meal? Unstable blood sugar sends conflicting messages to the brain about the need for food.
- Are you experiencing any weakness or fatigue? Do you feel strong enough to do all the activities you were easily able to complete before your symptoms? How do you feel after eating a meal? Stronger, weaker or the same? When sugar can't get into cells to energize them, kidneys have to work overtime to remove the extra sugar. This can cause weakness and fatigue.
- Do you feel a tingling or numbness that feels like pins and needles or burning in your feet when you wake up? Extra sugar in the blood can damage nerve-endings, especially those nerves located furtherest from the spinal cord like the feet.
- How is your vision? Are you experiencing any blurriness? When does it happen? At different times during the day, or does it stay the same? Is it getting worse? Sugar lingering in the blood can cause swelling in the lens in the eye making it difficult to focus. When sugar is really high, vision blurs, when sugar drops again it clears.
- How does your skin feel to you? Normal, or have you felt itchy and been scratching more than usual? Have you noticed a lot of dry skin even after increasing your water intake? Poor circulation paired with the loss of fluids (from frequent urination) can cause the skin to dry out. Dry skin leads to itchy skin.
- Have you noticed any slow healing wounds and increased skin infections? Any paper cuts, bumps and bruises that take more than a few days to go away? Any cuts that scab over repeatedly or wounds that last weeks to months before healing? Lingering sugar in the blood causes damage to veins and arteries disrupting circulation. Without proper blood flow, it takes longer for cuts and bruises to heal and the patient is more prone to skin infections.
- Any big mood swings lately? Have you or your family noticed that you are more irritable than usual? Have you had strong feelings of anxiety or depression? How are you sleeping at night? Unstable blood sugar has been known to cause mood disorders such as irritability, anxiety and worry. High blood sugar also mimics symptoms of depression; having low energy drive and wanting to stay in bed.
- Have you experienced urinary tract infection or yeast infection on a regular basis? High sugar levels within the urine breed bacteria and yeast near the genitalia. Urinary tract infections (UTI) cause symptoms of burning sensation during urination and cloudy, dark or off-smelling urine. Yeast infections cause itching, burning and discharge. People with diabetes are twice as likely to suffer from these types of infections.
Once the Arterial Doppler Test is completed, if findings validate diminished blood flow then our diabetic foot doctor will refer you to an interventional vascular specialist to restore blood flow to your foot and ankle.
Any patient with undiagnosed diabetes suspected of being diabetic from their medical exam will be referred to their primary care physician for a full workup.
Indicator 2. Have you had a recent (within the last 6 months) blood test checking HgA1c levels? If yes, is your current HgA1c over 8.0?
Hemaglobin A1c is a common blood test that measures average blood sugar levels over the last three months and is used to diagnose type1 and type 2 diabetes.
If you have had a recent HgA1c and it is above normal range then you have probably already been educated somewhat about the risks for and symptoms of diabetic foot complications when blood sugar is not controlled. We know that you are here to get into a diabetic foot care program with a structured care plan.
If you have not been diagnosed with diabetes and have not had a recent HgA1c then our diabetic foot specialist will order one.
This test is very important for patients who present with the above symptoms because blood glucose control is necessary for diabetic ulcer prevention and wound healing. When HgA1c is high, your body's ability to produce collagen to heal an ulceration is dramatically diminished. Controlling blood glucose with proper nutrition, exercise, oral diabetes medication and insulin are essential to prevent ulceration and also to allow for optimal wound healing in the event of skin breakdown.
When HgA1c is 8.0 and higher fibroblast, a type of cell that contributes to the formation of connective tissue and secretes collagen proteins to help heal, don't work well. In this case, the wound takes longer to heal or doesn't heal at all.
Indicator 3. Are there any prolonged pressure points on your foot and ankle?
A critical step in preventing and treating diabetic foot wounds is to off-load pressure being put on the skin and soft tissues from a structural abnormality (a prominent bone) rubbing repeatedly within the shoe. Common pressure points at risk are underneath the metatarsal heads, on top of the toes or foot, and at the end of the toes or on the ankle bone.
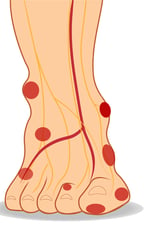

Common pressure points
The micro repetitive trauma from the bony prominence results in skin breakdown over time. Once skin integrity is compromised, bacteria can get into the open wound and cause foot infection. If diabetic foot infection isn't diagnosed and treated quickly the infection can spread to the bone. Once bone is infected, treatment includes hospitalization for IV antibiotic, surgical intervention and ultimately amputation if the bone infection is not caught in time.
For these reasons, identifying any bony prominence and off-loading those areas on the initial prevention visit can have a very positive impact on avoiding diabetic foot wounds later.
Indicator 4. Are there any beginning signs of skin breakdown (redness, warmth, callus or abrasion)?
If your circulation is good, your HgA1c is normal, you are wearing shoes and insoles that off-load any pressure points, then your doctor looks for signs of musculoskeletal deformity producing a prominent corn or callus putting you at risk for skin breakdown.
If your doctor finds a deformity producing a prominent corn or callus, then baseline digital x-rays will be taken in order to compare the progressing severity over the next few years. X-ray can be a long-term predictor of a potential pressure site which could result in an ulceration if not addressed.
Indicator 5. How is your nutritional status? Did you have a blood test to check your serum albumin level during your last check-up with your primary care physician?
If the patient has not had nutritional status checked recently (within the last 6 months) then our diabetic foot doctor will order this blood test. Nutritional status is crucial for bone, blood vessel, tendon, ligament and soft tissue health and repair. Malnutrition is highly prevalent and overlooked in patients with diabetes and chronic wounds. Normal serum albumin level needs to be within normal range of 3.4 to 5.4 g/dl (34 to 54 g/L).
We want our preventative program to head off complications so we want to get a good head start on improving any nutritional deficits that might leave you vulnerable to attack by this disease.
Education And Compliance Are Key To Prevention
That's why we put such a big focus on patient and family education regarding diabetic foot care, ulcer prevention and wound healing. Knowledge about prevention, the proper care of even very minor wounds and the risk of recurrence is necessary to safeguard quality of life for the patient.
Avoiding or reducing hospital visits and increasing ulcer-free duration is our goal. Long-term surveillance, integration of treatment among healthcare providers and information sharing can maximize the results of the care provided.
Early diagnosis is key. So is having an interdisciplinary team of specialists monitoring your health status through diabetic wellness and prevention visits. If you have this in place then you are taking the very best course of action you can to prevent complications of diabetic foot problems.
In next week's article we will discuss treatment steps that can be taken to get an open and infected diabetic foot wound to heal as quickly as possible.


